
EPFLSTILOBMarcel LeuteneggerAbout
Laser Doppler imaging
Mapping the microcirculation
 |
EPFLSTILOBMarcel LeuteneggerAbout Laser Doppler imaging Mapping the microcirculation |
|---|
Laser Doppler imaging (LDI) is a non-invasive imaging modality compatible with classical medical instrumentation, where discomfort and risk to patients is minimized. LDI is able to monitor the blood perfusion in dermal tissue, for instance the microcirculation in skin. Full field LDI of dermal blood flow has gained much interest in recent years, because anomalously altered peripheral blood flow provides an easily accessible indicator for various health disorders [1], e.g. altered vasodilation in the case of diabetes [2], reduced blood flow in the case of smokers [3], inflammatory responses in the case of rheumatic diseases [4] or, presumably, altered perfusion in the brain due to Alzheimer disease which might be evidenced in the retina [5,6].
In the beginning, scanning LDI instruments were developed [7,8]. These instruments assess blood perfusion over large areas and find widespread application in burn assessment and wound healing [9-12]. However, mapping the blood flow with a scanning LDI instrument typically takes minutes; often requiring the subject to be stabilized during the imaging process. An array based LDI approach using a fast CMOS camera for full field perfusion imaging was introduced in 2002 by Serov et al. [13]. This initial work triggered the development of several full field LDI instruments with ever increasing performance [14,15]. In 2009, Draijer et al. [16] presented the Twente optical perfusion camera, which represented a further essential step towards real-time full field LDI. Recently, the first integrated real-time full field LDI instruments became available as a research instrument in 2010, as well as a fully equipped instrument for medical applications in 2011.
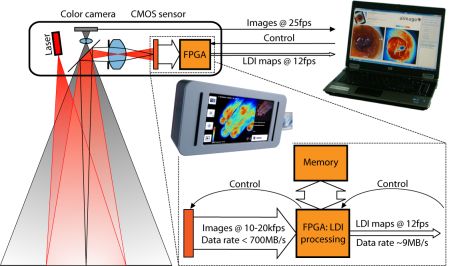
Figure 1: Aïmago laser Doppler imager developed in close cooperation with our laboratory.
The instruments incorporate a high-speed CMOS camera chip and a powerful FPGA chip for controlling the CMOS sensor and for real-time processing of the captured images. The resulting blood perfusion, erythrocyte concentration and intensity maps are then sent to a host computer for further analysis. The performance of the instrument allows continuous video-rate monitoring of blood flow.
We present a full field laser Doppler imaging instrument, which enables real-time in vivo assessment of blood flow in dermal tissue and skin. Our instrument monitors the blood perfusion in an area of about 50cm2 with 480×480 pixels per frame at a rate of up to 14 frames per second [a]. Smaller frames can be monitored at much higher frame rates. We recorded the microcirculation in healthy skin before, during and after arterial occlusion. In initial clinical case studies, we imaged the microcirculation in burned skin and monitored the recovery of blood flow in a skin flap during reconstructive surgery indicating the high potential of LDI for clinical applications. Small animal imaging in mouse ears clearly revealed the network of blood vessels and the corresponding blood perfusion.
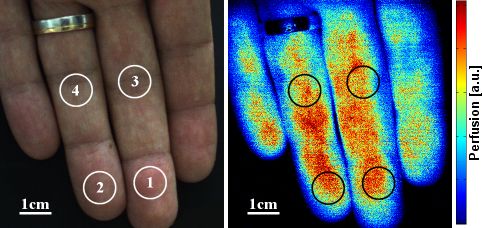
Figure 2: Color image of fingertips and color-coded blood perfusion map. Captured video sequences showing the start of the arterial occlusion and the overshoot after release. Both resized to 50% of the original images.
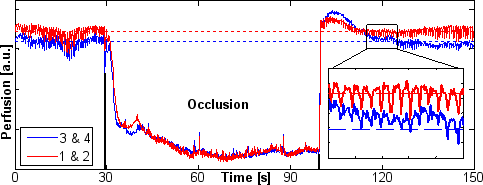
Figure 3: Blood perfusion in the encircled regions on the fingers. During the arterial occlusion, the blood perfusion drops and motion artifacts (spikes) become more clearly visible. The heartbeat is shown for a 10s interval when the blood perfusion returned to normal.
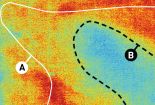
The identification and accurate location of centers of brain activity are vital both in neuro-surgery and brain research. We aime to provide a non-invasive, non-contact and accurate imaging of brain function intraoperatively. In a preliminary study, a full field Laser Doppler imager was developed and integrated within the surgical microscope. Perfusion images of the cortical surface were acquired during awake surgery whilst the patient performed a predetermined task. Active brain regions showed an ~10% change of blood perfusion related to the stimulation protocol, which lead to intraoperative functional brain maps of strong statistical significance [b]. The activity maps correlated well with the preoperative functional MRI and intraoperative cortical electro-stimulation. These initial results demonstrate the feasibility of LDI as an appropriate technique for intraoperative brain activity mapping.
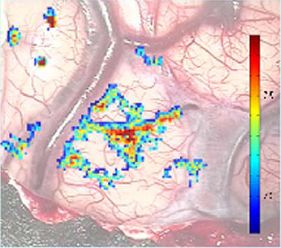
Figure 4: Functional brain map showing the active motor cortex when the patient was tapping with his fingers. The colors indicate the statistical significance of the correlation between the patients activity and the blood perfusion in the brain.
This work was supported by the Commission for Technology and Innovation (CTI project no. 10218.1 PFLS-LS), Switzerland. T. Lasser, M. André, M. Leutenegger and A. Lopez are shareholders and cofounders of Aïmago. P. Lasser is a shareholder of Aïmago.
© 2011 École Polytechnique Fédérale de Lausanne